‘A scary hearty meal.’
A 50 year old woman had decided to go to bed just then she had felt a tingling sensation in the palms of her hands. It was all too familiar, in the past eight years she had it twice. It felt like a strange itch in her hands and sometimes her feet. Each time this had occurred there was a terrible feeling of her throat closing. With a lot of effort, she drove herself to her sister’s house; and her sister accommodated her in the car and drove her to the hospital. She struggled to breathe; letting in some air by rolling down the car windows might be of some benefit or so she thought. Black spots swam about in front of her eyes. She persevered herself to keep up till they reached the hospital; an unfortunate malady all patients go through.
She was admitted to the emergency room by her sister. She dropped into the wheelchair, before that she shared of her feeling like she can’t breathe and threw off her sweatshirt; she felt it was too tight all of a sudden. Her blood pressure was alarmingly low and her heart was racing. This allergic reaction had occurred twice before but not of such intense severity. Upon her own research, she had stumbled upon anaphylactic shock. The medication resolved the symptoms. An overnight hospital stay and few hours more made it clear that the episode was over. She had decided to return to her mother’s house. She made sure to see a local allergy specialist right away. It took the allergy specialist two hours to go through it all. She knew that all her exposures weren’t new of any kind. The allergist couldn’t pinpoint the exact cause. The most common was known to be food in adults.
After reaching back home from her mother’s
She was now constantly in fear of what harm the food she consumed would do to her. This was every night she went to bed. A bottle of Benadryl and an Epi pen to console her woes. Her fear drove to feel the need to be inches closer to the hospital. The next 10 months followed with a case of gastroenteritis due to salmonella for which she was treated with antibiotics for. Her earlier meals consisted of clear fluids and nothing else. It took her a while to move on to a beef brisket meal with potatoes and carrots. It smelled good but she had no appetite. Yet, she took few bites.
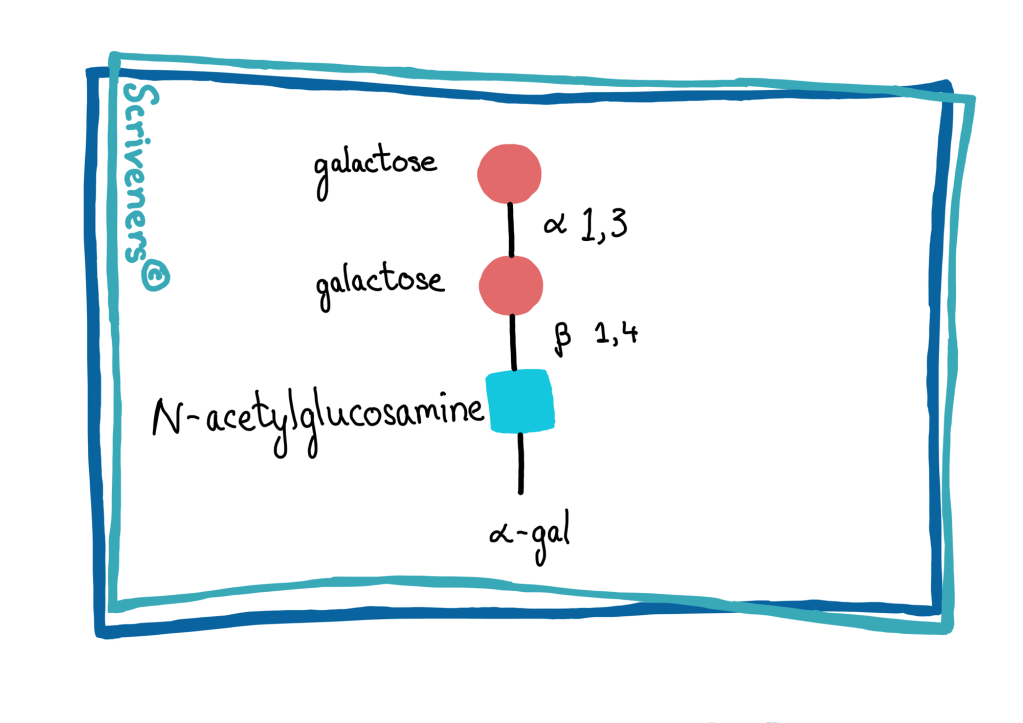
A couple of hours later, she had a strange itch on the top of her head. She ran across the hallway to look for a nurse still grabbing tight onto her IV fluid stand and bag dripping into her systems. She, with confidence told them she’s having an allergy attack instead of a panic attack. The hospital staff helped her go back to bed and equipped her with oxygen, Benadryl and the steroids. The doctors were still sceptical of her claim, they think it was an antibiotic allergy. Except here, she wasn’t on any antibiotics, a nurse suggested her to check if she had an allergy, the one caused by ticks biting, perhaps it’s that. A diagnosis of MMA-Mammalian Meat Allergy was confirmed on a blood test that showed antibodies against alpha-gel. After a month, the tests had confirmed that she’s heavily allergic to galactose-α-1,3-galactose.
Diane Cymerman, an allergist called up the patient with the bad news. She had to avoid eating meat from mammals—and everything derived from them, including Jell-O and other foods and medications made from gelatin.
Clinical allergy specialists in Australia were the first to describe the link existing between tick bites and the development of mammalian meat allergy. This association was confirmed by researchers on all six continents. The proteins in the tick saliva are the allergens that cause the tick allergy. The allergic response doesn’t necessarily occur at the time of the tick bite, it can happen any time after the tick bites and this includes months or even years after the initial bite. Any life stages of life cycle of the tick bite can create the immune response. Alpha-gal is a sugar molecule present in all mammals except humans. Symptoms can range from gut symptoms to life-threatening anaphylaxis. Irritable bowel syndrome is reported to be the common gastrointestinal symptoms in patients with MMA. Management includes avoiding the confirmed food allergens, knowledge of its signs and symptoms and how to be ready when a reaction occurs and carrying an adrenaline injector and the ASCIA Action Plan at all times as its potentially life-threatening.
Credit: All clinical cases from Diagnosis: Solving the Most Baffling Medical Mysteries-Lisa Sanders. (Cases go in no particular order!)
Dr Lisa’s website: https://www.nytimes.com/by/lisa-sanders-md
Sources: https://www.allergy.org.au/patients/food-allergy/mammalian-meat-tick-faq?highlight=WyJhcyJd
https://pediatric.testcatalog.org/show/APGAL