‘A Hit of that Wonderful Molly’
A 20-year-old young woman lay on the stretcher, with her eyes closed while her arms and legs were in a restless motion. She was now clearly pale and unresponsive. Her mother stood at the doorway, petrified of what was yet to come, she approached her daughter’s bedside and whispered, “What have you done, my little girl?” Sadly, the young woman was unaware of her surroundings, the fact that her mother was present in the ER of the Upstate University Hospital, Syracuse, New York. The only thing the ER doctors could inform her was that her daughter was dropped off early morning by a young man around the same age.
The triage nurse was told that he had gone to a concert with the unresponsive woman the night before. Though they were separated by the time evening came, she appeared to be happy, seemingly euphoric. It was the next morning that started to get worrisome, she was still on his couch, she slept but that didn’t change much as she began to vomit and was incontinent. Her mother felt guilty for not being there for her daughter but was also angry, hurt that she had been trying to cell her home, and her daughter had not called back. The night before she had not reached home as promised. At six o’clock in the morning she drove to the apartment of her friends that was the first thing she had resorted to do and got done.
Her mother told the man to let her daughter know that she was in big trouble for the recklessness of the situation but somewhere, then, her mind was filled with anxious thoughts; why was it not her who had to go and check up on her? And how she could’ve left her there? What moral ill has this man caused to her daughter bringing her to the hospital only to leave her in the ER for treatment rather than being by her side?
The ER doctor Lauren Pipas found that she was unable to respond to her name, answer any simple questions or follow on the commands. A sternal rub-to elicit a pain response that would help assess her consciousness was used. She moaned in response, her eyes remained closed and there was no fever and her heart was beating normally. A patient of this age who presented with no obvious illness and was unresponsive probably meant that the likely culprit was a drug intoxication or overdose.
Dr Pipas ordered for a urine drug screen (UDS); it’s a 10-panel drug test to figure out which of the commonly abused drugs would be in her system. It can detect traces of cannabis, cocaine, opioids, benzodiazepines, amphetamines, barbiturates, and for individual drugs such as phencyclidine (PCP), or angel dust, MDMA (ecstasy), methaqualone (Quaaludes), propoxyphene. Her blood was also tested for acetaminophen and salicylates; an active ingredient in aspirin. The urinary incontinence that the young man said could suggest a seizure possibly. So, the ER doctor ordered for an EKG, a chest X-ray, a head CT and for the routine labs as well that included a blood count and a chemistry test. She also tested for thyroid disease and pregnancy that were common the ER for women. The EKG and CT came back normal.

The urine test came back positive for amphetamines and her serum sodium was dangerously low; this low limit must be an explanation for the seizures she thought.
Amfetamines cause wakefulness, excessive activity, paranoia, hallucinations, and hypertension followed by exhaustion, convulsions, hyperthermia, and coma. The early stages can be controlled by diazepam or lorazepam; advice should be sought from the National Poisons Information Service on the management of hypertension. Later, tepid sponging, anticonvulsants, and artificial respiration may be needed.
First developed in 1914 as an appetite suppressant, MDMA found use as a psychotherapeutic agent during the 1970s. However, its potential for abuse was quickly recognized, leading government agencies to place tight restrictions on its use. MDMA is a commonly abused drug, particularly among young partygoers at electronic dance music venues, including dance clubs and festivals. Typical effects include feelings of euphoria, wakefulness, intimacy, excitement, and disinhibition. Ecstasy (methylenedioxymethamphetamine, MDMA) may cause severe reactions, even at doses that were previously tolerated. The most serious effects are delirium, coma, convulsions, ventricular arrhythmias, hyperthermia, rhabdomyolysis, acute renal failure, acute hepatitis, disseminated intravascular coagulation, adult respiratory distress syndrome, hyperreflexia, hypotension and intracerebral haemorrhage; hyponatraemia has also been associated with ecstasy use.
Treatment of methylenedioxymethamphetamine poisoning is supportive with diazepam to control severe agitation or persistent convulsions and close monitoring including ECG. Self-induced water intoxication should be considered in patients with ecstasy poisoning. It falls under Class A and Schedule 1.
It would also explain why she remained unconscious. Here, another question arose as to why it was so low, her sodium levels?
This could be answered once the young woman had stabilised. She ordered for a sodium solution that would replace the essential electrolytes and a sedative for her agitation was given.
A team from the intensive care unit was called. Shaun Cole, a fourth-year medical student was the first to arrive. He reviewed the patient’s chart and eyeballed the patient. What he observed was that the patient’s restless movements had stopped but she was still responsive only to pain.
He continued to ask questions to her parents and her brother over the events that have happened within the last 24 hours. She was a good student and had just been out with some friends, she would work at a local restaurant for an alternate source of income which meant that she didn’t have much time for anything really.
Had she used drugs before?
Just the alcohol. And nothing else.
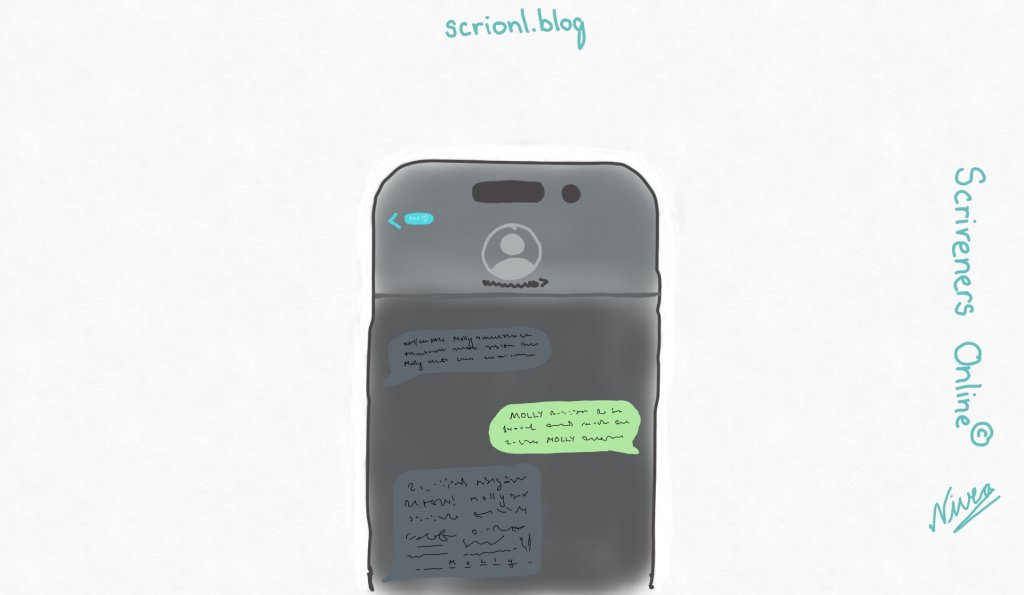
Her brother rummaged through her belongings, finding her cell phone, when Cole looked through it. He saw references on ‘Molly’ in her instant messaging. A quick Google search would reveal that ‘Molly’ was another name for ecstasy, it’s another amphetamine derived drug. It was often used at concerts and raves. That afternoon, Cole spent his time searching the link.
Why would a woman have such low sodium if it was a first-time drug use by incidence?
The drug promotes water retention, diluting the sodium in the body, and case reports show that it was not linked to higher doses but to someone who has used the drug before like some kind of indicator. It’s a dangerous side effect and one out of five who developed hyponatremia had died because of this incremental drug use. The patient unfortunately woke up a week later, and it was obvious that her brain was injured by the jumbling and slow speech and the impaired vision, she had to learn to read and write all over again.
She spent the next several months regaining all of her losses and had somehow managed to graduate one semester behind her classmates. She had taken ecstasy once before. That day, when she was admitted, she was neglected for a few hours. Were her friends fearing at the thought of getting caught? Her mother decides to do something about it, with the state senator’s help, she lobbied for the passage of the ‘Good Samaritan Law’ in the New York State.
Unintentional drug overdose is a leading cause of preventable death in the United States. Some states have enacted “Good Samaritan” laws that create immunities or other legal protections for people who call for help in the event of an overdose to encourage and protect bystanders who may otherwise not be willing to call for fear of being arrested for drug-related crimes. The protection afforded by these laws varies from state to state. Some states have comprehensive Good Samaritan overdose prevention laws that provide broad protection, while others have passed laws that consider seeking medical assistance for a person experiencing an overdose as an affirmative defense, or as a mitigating factor during sentencing.
Clinician and patient interest in MDMA as a potential therapy has increased and research and experimental use of MDMA to treat several psychiatric disorders (eg, post-traumatic stress) continues. In 2024, an application for US Food and Drug Administration (FDA) approval of MDMA as a therapy for post-traumatic stress disorder was rejected. The rejection was based on concerns over the quality of studies presented in support, several of which have been retracted, but use of MDMA for purported psychological benefit continues.
Source;
BNF 85 & Diagnosis: Solving the Most Baffling Medical Mysteries-Lisa Sanders. (Cases go in no particular order!)
https://www.uptodate.com/contents/302#H1
https://substanceabusepolicy.biomedcentral.com/articles/10.1186/s13011-020-00295-1
https://www.medicalnewstoday.com/articles/326305#which-drugs-are-tested-for
https://pdaps.org/datasets/good-samaritan-overdose-laws-1501695153