A low cost tele-ausccultation system which comprises an electronic stethhoscope with a Bluetooth link to an electronic health reecord server.
Tele-auscultation is a diagnostic method that combines face-to-face auscultation with the use of information and communication technologies to remotely transmit auscultation records for diagnostic purposes or for patient follow-up. It is based on the use of a connected electronic stethoscope. The telemedicine systems enable cardiac and respiratory sound listening wirelessly.
Several studies have shown that this approach can be effectively implemented to diagnose heart diseases[15] [20–22].
During auscultation, the fact that a physician has access to a patient’s clinical information improves decision-making (diagnostic, therapeutic, etc.) [23]. In addition, the electronic stethoscope is a sensitive tool and can perceive sounds that are not perceptible when using a conventional stethoscope.
Challenges & Feedback
First, there is a lack of training and education in tele-auscultation. The introduction of this innovative approach (use of the electronic stethoscope and remote analysis), requires carrying out capacity building sessions beforehand, in order to give doctors all the skills they need to better appropriate the device. Given the similarities with face-to-face auscultation using a conventional stethoscope, we hypothesised that physicians’ appropriation of this digital-based or remote auscultation would be natural and intuitive.
In addition, there are artefacts that may compromise the digital-based or remote analysis of heart sound recordings. Comments were made by the various cardiologists on this subject. Subject to excellent suppression of ambient noise (and therefore better quality of heart sound recordings), a better agreement can be achieved between the conclusions from the face-to-face assessment of patients using the conventional stethoscope and the conclusions from the digital-based or remote assessment (teleauscultation) of heart sound recordings using the electronic stethoscope [24].
Finally, the residual variability between evaluators can also be explained by the difference in academic background and professional experience between cardiologists [21]. Experienced clinicians will tend to agree strongly when the diagnosis is simple and obvious [21]. However, an agreement between evaluators decreases significantly as the clinical signs to be evaluated become hard to perceive, as this requires the use of personal experience [21].
Although it is not the standard for the diagnosis of cardiac pathologies as it is for cardiac ultrasound, faceto-face auscultation remains the most cost-effective diagnostic method, especially in the context of resource-limited countries. It is a non-invasive and inexpensive diagnostic approach. With the continuous development of information and communication technologies, this face-to-face auscultation can now be done remotely (remote auscultation) through the use of electronic stethoscopes and telemedicine platforms.
Telemedicine Systems
Telemedicine systems are defined as electronic-transmission mediums that facilitate the exchange of medical information between individuals in geographically separate locations, utilizing telecommunications and medical device technology. (-AI Definition)
According to the Institute of Medicine, telemedicine is the use of electronic information and communications technology to provide and support health care when distance separates the participants [1].
As health care continues to overcome challenging ailments, the need for new techniques of patient monitoring has never been greater. Although there have been some important advances in monitoring technology, a thorough understanding of the application of available technology is just as important to safe, state-of-the-art patient care.
Patient Monitoring
Patient monitoring refers to the continuous observation and assessment of a patient’s physiological status, utilizing electronic medical records and prediction models to enhance sensitivity and specificity in detecting potential deterioration. It aims to facilitate timely interventions and improve clinical outcomes through effective alert systems and integration of telemedicine. (-AI Definition)
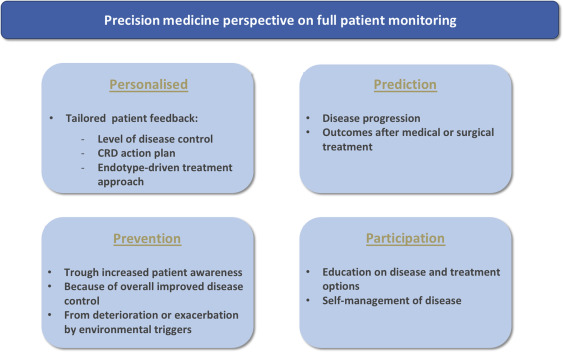
Full patient monitoring is the way forward towards delivery of healthcare according to the principles of precision medicine with:
•a personalized approach with tailored patient feedback based on real-time and real-life data of each individual patient. More concrete, which means that digital action plans need to be designed to guide disease management for each individual patient. Integration of results from biomarker analysis via point-of-care systems into digital health tolls will furthermore enable endotype-driven treatment of the patient.
•prediction of disease progression based on big data analysis of real-life data. As such, a benchmark might be created that allows comparison of the patients’ individual outcomes after medical or surgical treatment with subsequent tailored alerts when deviation against the benchmark is detected.
•prevention because of improved disease control by patients that actively take part in the management of their disease (self- management). Full patient monitoring will improve patient awareness on symptoms and compliance to treatment and as such might also improve treatment adherence and thereby improve disease control. Information on patients’ individual environmental exposure can be used for prediction of disease deterioration or exacerbation and subsequent adjustment of the disease management. As such deterioration or exacerbation might be prevented.
•increased patient participation in disease management via better educated patients and monitoring of their disease (Fig. 27.3).
Patient monitoring is critical in ICU environments. The purpose of monitoring equipment is to provide timely and maximum information. Good cognitive ergonomic design of monitoring equipment should serve to reduce human factor errors. Instrument-redesigning research is as important in reducing human errors as is focusing on organizational issues related to work. Innovative, targeted interventions for ICU alarms and their warnings have been previously suggested [83].
Patient monitoring is now an accepted standard in medical care to ensure that a patient’s condition can be evaluated over time and any deterioration identified quickly, enabling appropriate care to be instituted. (not AI)
What are the components of a monitoring device?
There are essentially four components to any monitoring device:
1)Sensor
2)Transduction
3)Amplification
4)Display
Point-of-care testing (PoCT)
The term PoCT refers to the performance of diagnostic tests carried out at or near a patient. In fact PoCT includes the invasive and non-invasive monitoring devices discussed already, but in general it is used to describe the rapid specific testing of bodily fluid at the bedside.
Wearable Sensor Technology
Wearable sensor technology enables recording and analyzing physical, chemical, and electrophysiological parameters in real-time and in a non-invasive way. The continuous monitoring of clinically relevant information aims at the prevention, treatment, and management of diseases and the well-being of the users. (not AI)
Wearable sensors can be considered in three categories: motion, biometric, and environmental sensors. For a wearable monitoring system to be practical it needs to meet several key criteria: to be non-invasive, intuitive to use, reliable, and provide relevant feedback to the wearer. Devices can be either attached directly to the skin using some form of adhesive, mechanically using a clip, strap or belt, or incorporated directly into clothing or shoes.
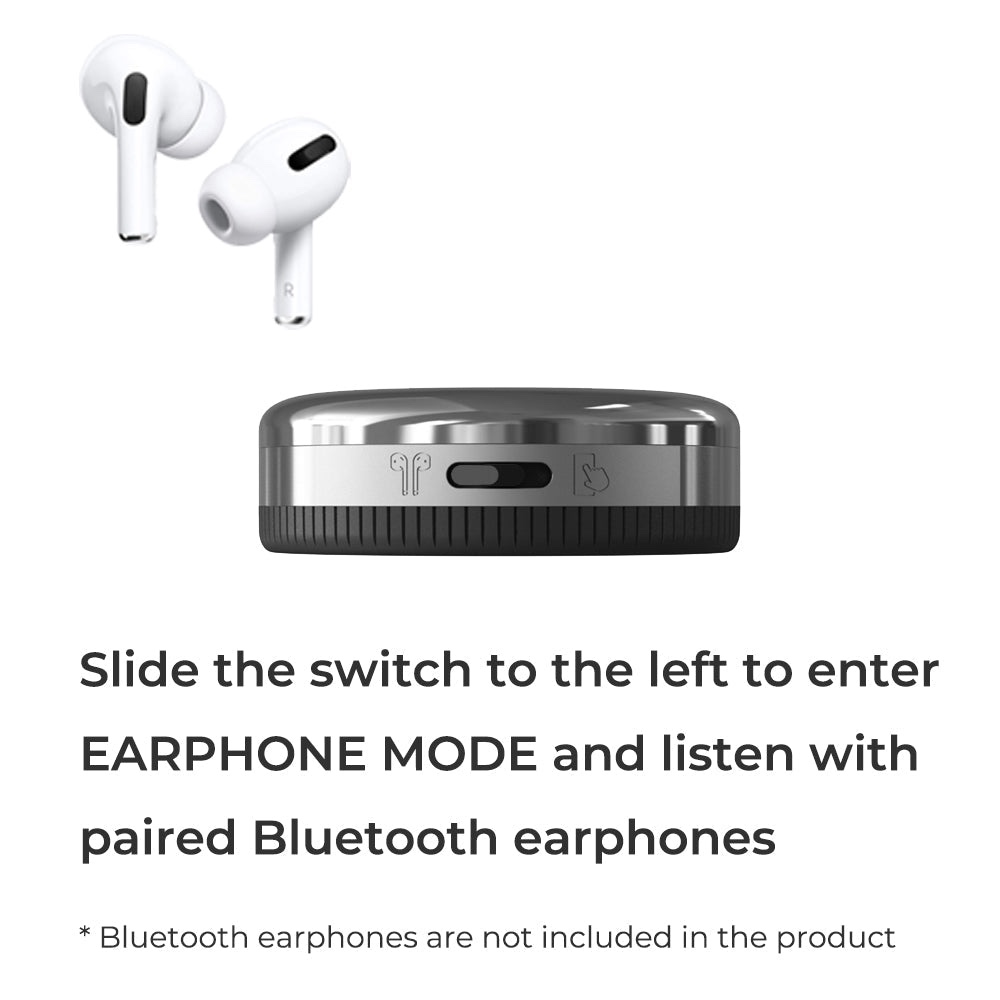
The Workings of a Tele-Auscultation
The present invention is to listen to and diagnose the biological signals of the internal organs of the human body that is the basis of the disease judgment, anytime, anywhere remote smart medical care system based on the digital remote stethoscope based on the remote medical examination system based on the smart phone and a method for operating the same, a digital stethoscope for digitally converting a stethoscope sound of a patient in a stethoscope process to generate stethoscope data, and a smartphone for storing the generated stethoscope data together with information of a patient name, a measurement part, and a measurement date. Doctor terminal to check the medical request by accessing the server, receive the requested stethoscope data, transmit the medical chart created by the doctor to the server, and provide a stethoscope for the remote patient, and the medical request chart
The user’s health status is displayed by the patient application of the smartphone by comparing the currently measured auscultation data with the standard waveform of the auscultation sound generated by the internal organs of the body according to the disease, and compared with the previously measured auscultation data transmitted from the server.
The request chart table storing the stethoscope data includes a chart number, a patient ID, a request date, a request file name, and request processing information in order to manage patient request information by connecting patient information. The medical data information table (Medical DataInfo) is composed of a data number, patient ID, measurement date, measurement site, and file name to connect the patient information to manage the stethoscope data for each patient. The patient table and the doctor table are composed of server login-related information including personal ID and password and personal identification information in order to manage personal information of the patient and the doctor.
Findings of Stemoscope
For murmurs detection, the in-person auscultation agreement between Stemoscope and the acoustic stethoscope was 91% (p=0.67). The agreement between Stemoscope tele-auscultation and the acoustic stethoscope in-person auscultation was 90% (p=0.32). When using the echocardiographic fndings as the reference, the agreement between Stemoscope (tele-auscultation) and the acoustic stethoscope (in-person auscultation) was 89% vs. 86% (p=1.00). The system evaluated by ten cardiologists is considered easy to use, and most of them would consider using it in a telemedical setting.
Conclusion: In-person auscultation and tele-auscultation by the Stemoscope are in good agreement with manual acoustic auscultation. The Stemoscope is a helpful heart murmur screening tool at a distance and can be used in telemedicine.





Is this the newer and improved digital upgrade of the conventional stethoscope? And more importantly is it meant to stay?
Game-changer! Isn’t it?!
If you are interested in buying a stemoscope; here’s the link! 😉
Sources:
https://www.sciencedirect.com/topics/engineering/telemedicine-system
https://www.sciencedirect.com/science/article/abs/pii/S0263931919301103
https://www.sciencedirect.com/topics/medicine-and-dentistry/wearable-sensor