Restoring impairing blindness and repurposing the old techniques…
“It’s incredible, it’s life-changing, it’s given me everything back. It was challenging. I couldn’t see to get around my house, I found it incredibly tough to get outside, How am I gonna see my child when he runs off?”
Nicki Guy
Hypotony is a rare and untreatable condition and clinical researchers at UCL alongside Moorfields Eye Hospital have uncovered a way to do so.
There’s a fluid in the eye that helps maintain normal eye pressure. The standard treatment for this in practice would be to fill them with silicone oil. Though it has its benefits, it can lead to toxicity and make it visually difficult to see. The data published today in the British Jornal of Ophthalmology indicates that ocular injections containing HPMC (hydroxypropyl methylcellulose) – a low-cost gel used in most eye surgery – can be safely used to increase the volume of eyes with hypotony, increasing both their size and pressure.
This study is a prospective interventional case series. Eight patients with chronic structural hypotony for more than 3 months, defined by an intraocular pressure (IOP) of <6.5 mm Hg. All patients had evidence of visual potential, clear cornea and a clear visual axis.Patients received multiple intravitreal HPMC injections (70 µL–1400 µL), administered every 2–4 weeks until either pre-morbid axial length was achieved, an IOP of 10–15 mm Hg was sustained for 4 weeks without signs of hypotony, or axial length of the contralateral eye was reached. They were followed up for 12 months after the first intravitreal injection.
This is the first case series to use a structured protocol for intravitreal HPMC in chronic hypotony management. The treatment improved vision and restored ocular anatomy, showing promise for managing structural hypotony in eyes with visual potential.
Nicki’s sight issues began shortly after the birth of her son, when she was diagnosed with uveitis. For several years, she lived symptom-free, until cataracts and further complications began affecting her eyes. Multiple treatments were attempted, including the use of steroids and silicone oil. While some offered temporary relief, others led to sudden drops in pressure or even complete loss of vision.
Losing vision had been frightening, but it also pushed Nicki to find out about treatment options and cutting-edge research, saying: “After I lost vision in my left eye, I thought, ‘there has to be something else we can try’. It felt good that I’d been able to advocate for myself, like they understood my concerns.”
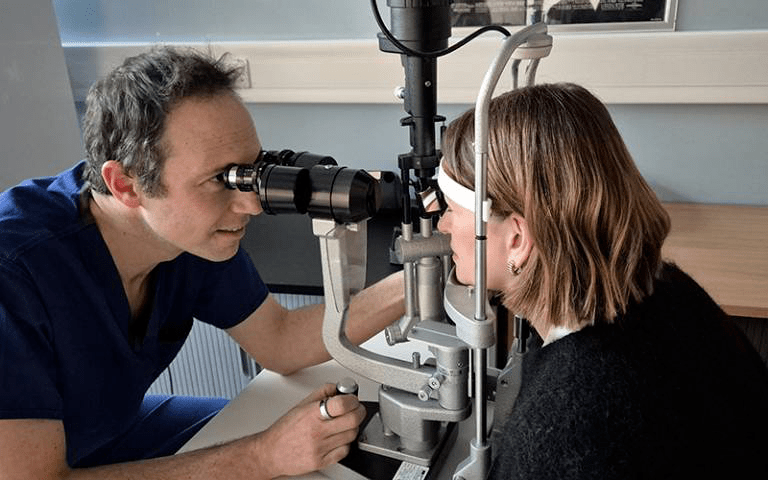
Her turning point came when her consultants at Moorfields began exploring an alternative to silicone oil. Encouraged by her persistence, they trialled a new approach – an injection of clear gel designed to support pressure and restore function.
Reflecting on that moment, Nicki said: “We went ahead and, as the pressure improved, my vision started to come back. It was incredible!
“I want to keep my eyesight as long as I can, and this gives me that hope, as my sight has slowly returned. The progress I’ve made feels extraordinary, especially knowing that patients before me have faced irreversible sight loss.
“I remember seeing Mr Petrushkin and him saying, ‘Before this treatment, people were going blind.’ It’s incredible to know that people are regaining vision. I highly recommend this treatment. Giving people their sight back is something special.”
Moorfields consultant ophthalmologist Harry Petrushkin, lead author of the study, said: “We are excited that this simple treatment has proved so effective for patients with this rare condition. This is the start of a process of understanding more about the balance of fluid inside the eye, leading to improved care for our patients.”
Co-author Professor Gus Gazzard (UCL Institute of Ophthalmology and Moorfields Eye Hospital) commented: “This is a truly transformative new therapy that brings hope to patients otherwise without options, for what was previously an untreatable blinding and disfiguring condition. This robust proof of principle study has already exceeded my hopes of what sight recovery might be achievable.
“I hope that we shall be able to make it more widely available to more patients very soon, but of course these are early steps, and more hard work will be needed, not least to raise the funds needed to optimise this treatment.”
The Moorfields clinic integrates structured clinical assessment and collaboration with bioengineers at the UCL Department of Mechanical Engineering to understand the drivers of chronic low intraocular pressure. The project has been supported by the UCL Institute of Healthcare Engineering summer studentship programme, with UCL Mechanical Engineering students working alongside academics to help develop a computational model that aids clinical understanding of the procedure.
Sources:
https://www.ucl.ac.uk/news/2026/jan/world-first-project-shows-great-promise-treat-low-eye-pressure
https://bjo.bmj.com/content/early/2026/01/04/bjo-2025-327866