Martha’s Vineyard takes an hour drive from Boston. It’s a popular vacation spot and artists, politicians and actors call it a home for the summertime. The Island of Martha’s Vineyard is New England’s largest island. Legend has it that the Vineyard was given its name in 1602 by Bartholomew Gosnold who named it for one of his daughters and the wild grapes he found there. The Island is nine miles wide and 23 miles long at its farthest points. The total land area is approximately 100 square miles with a total of 124.6 miles of tidal shoreline. In the summer of 2000s, there were a few Tularaemia cases that shot up. On June 18th 2000, Patrick Ryer a landscaper by profession, as the morning hours passed, he started to feel lethargic and run-down. His profession despite being physically demanding was enjoyable to him. He felt that he might have a case of the flu and decided to take the rest of the day off.
Evening approached and he was too weak too pick up the call. His girlfriend tried to reach him. Unanswered calls prompted her to drive to his house. Paula Stroel knew he was in this state for several days. As she entered his home, she noticed that he was worse than she expected him to be. Patrick was pale, shaking with fever and sweating uncontrollably. “Please let me take your temperature.” Paula says. On touch, his skin was getting warmer and warmer she recalls. His fever had a temperature that mildly confused her and he had a temperature of 106 degrees on her second check.
She knew that he needed immediate hospital care. So she lifted him up herself and took him to the hospital right away, it was the quickest she could be at this point. On their way to the hospital, Patrick was sounding incoherent. He seemed to be getting progressively worse. She continues, “He started talking under his breath and she didn’t even know what he’s saying half the time.”
By the time they reached Martha’s Vineyard Hospital, Patrick could no longer speak. “He got really quiet and it scared me even more.”
A nurse took his vital signs in the examination room, wherein his temperature was still at 105.9 degrees. He was rushed by the ER staff into intensive care, they administered fluids and if he wasn’t stabilised the fever could result in seizures, brain damage and even organ failure.
On listening for his sounds with the bell on his chest, the doctor interpreted sounds reminiscent of pneumonia. Inflamed lung tissue on the X-rays confirmed the diagnosis.
There was one problem though. Doctors were clueless when it comes to the causative agent.
Lab technicians analysed his blood and urine samples. One clue was that there was a high white blood cell count meaning that the body was fighting a bacterial infection. Unfortunately, the hospital on such a small island didn’t have the facilities to further test the samples.
This was something the Massachusetts State Lab could handle. The results would take several days. He was started on intravenous antibiotics that would aid his body in fighting off the infection. The medication’s effect would take upto 24-48 hours to work its magic. “It was amazing how, how weak he was. How there wasn’t much left of him. How he was just lying there, I cried… I really didn’t think he was going to survive the whole evening.”
At night, the ER physician alerted the hospital’s infectious disease specialist Dr Dennis Hoak, on questioning his girlfriend he suspected that the infection occurred outside.
“Martha’s Vineyard has this unusual collection of tick-borne diseases. Tularaemia, babesiosis, ehrlichiosis, Rocky Mountain spotted fever, and Lyme disease and the local physicians knowing that we have this collection of diseases, know that they really have to think about it (in any fever that comes through the summer).
Dr Hoak believed that Patrick was suffering from a tick-borne illness. But he had to wait for the lab results to confirm. Another confirmed case was a boy named Chris whose parents were worried about.
Two cases in the summer within a week of each other was unusual. The doctor asked Chris if he had suffered from an insect bite recently. His parents couldn’t recall anything of such, this was all until his lab results came back. The exact cause of his illness remained a mystery, all the doctor could do was prescribe multiple antibiotics.
Dr Hoak was troubled by the increase in pneumonia cases in the summer months. He thinks that the clues lead to a possible tick-borne illness as there are many ticks lurking around Martha’s Vineyard. Dr Sam Telford, a Parasitologist studies the questions on ‘How many ticks are there each month?’
‘How many cases do we see each month of any of the tick-borne diseases?’
‘Can we ultimately find out if the weather is favourable for a tick-transmitted disease/tick transmission to occur?’
So far there was no notes of anything unusual.
Still weak and dazed from the illness, Patrick could not remember anything unusual. While going through hospital records, Dr Hoak found a third case, a man in his late 40s named John Franklin who had contracted pneumonia two weeks earlier.
A colour change was what lab technicians looked for at the Massachusetts Department of Public Health and it indicates the presence of the bodily response of antibodies fighting off the infections and is a big clue in these types of cases. The samples were taken from all the three patients. All of three patients blood tested positive for Tularaemia. It’s a rare and deadly bacterial infection that’s widespread among rabbits and rodents. It’s life threatening when it’s affecting the lungs. But it doesn’t always kill the small mammals that it’s closely associated with!
The doctors were concerned as 20 out of the 200 were deadly. They contacted the CDC. Dr Katherine Feldman, an epidemiologist was alarmed. “The organism that causes Tularemia is considered a category A Bioterrorist agent. Category A means high priority. And it’s gets that classification because it’s potentially easy to disseminate, it has a high mortality if untreated, it can cause 60% mortality in folks who have the infection. And it has the potential to cause widespread panic.”
Clinical investigators were hot on the case. All they knew was that it didn’t spread person to person.
“If someone gets the pneumonia form of plague, it can be transmitted from person to person by coughing.”
The CDC was notified of another case of 58 year old Neil Kravitz. He owned a cottage on the island and often spent weekends there.
Their first step was to determine the scope of the problem, they needed to know if any previous cases of Tularaemia had gone unnoticed or misdiagnosed. Donna Stiles-Enos, an Infection Control Nurse adds, “We reviewed maybe around 40 charts at that time and found that none of them fit the criteria for tularemia, so really we do not believe that that there were any cases before those initial cases.” Besides the patients symptoms and time spent outdoors there were a few similarities. Clinical Investigators went back to find the first confirmed case of tularemia.
There are 7 clinical syndromes associated with tularaemia.
Clinical manifestations vary by the type of exposure to the organism.
It enters the body by
- Ingestion of contaminated food or water
- Bite of an infected arthropod vector (ticks, deer flies, fleas)
- Inhalation
- Direct contact with infected tissues or material
The causative organism, F. tularensis, is a small, pleomorphic, nonmotile, nonsporulating, aerobic, gram-negative bacillus.
The organism can penetrate apparently unbroken skin but may actually enter through microlesions.
Two types of F. tularensis cause most cases of tularemia:
- Type A: This type is a more virulent serotype for humans; it usually occurs in rabbits, hares, and rodents in the United States and Canada.
- Type B: This type usually causes a mild ulceroglandular infection and occurs in rodents and in aquatic environments throughout the Northern Hemisphere, including North America, Europe, and Asia.
Symptoms and Signs of Tularaemia
Onset of tularaemia is sudden, occurring 1 to 10 (usually 2 to 4) days after exposure, with headache, chills, nausea, vomiting, fever of 39.5 to 40° C, and severe prostration. Extreme weakness, recurring chills, and drenching sweats develop.
Within 24 to 48 hours, an inflamed papule appears at the site of exposure (finger, arm, eye, roof of the mouth), except in glandular or typhoidal tularemia. The papule rapidly becomes pustular and ulcerates, producing a clean ulcer crater with a scanty, thin, colorless exudate. Ulcers are usually single on the extremities but multiple in the mouth or eyes. Usually, only 1 eye is affected.
Regional lymph nodes enlarge and may suppurate and drain profusely.
A typhoid-like state frequently develops by the fifth day, and the patient may develop atypical pneumonia, sometimes accompanied by delirium.
Pneumonic tularaemia
Pneumonic tularaemia can occur after inhalation or by hematogenous spread from another type of tularaemia; it develops in 10 to 15% of ulceroglandular tularaemia cases and in about 50% of typhoidal tularaemia cases.
Although signs of consolidation are frequently present, reduced breath sounds and occasional rales may be the only physical findings in tularemic pneumonia. A dry, nonproductive cough is associated with a retrosternal burning sensation. A nonspecific roseola-like rash may appear at any stage of the disease. Splenomegaly and perisplenitis may occur.
In untreated cases, temperature remains elevated for 3 to 4 weeks and resolves gradually.
Mediastinitis, lung abscess, and meningitis are rare complications.
Diagnosis of Tularaemia
- Cultures
- Acute and convalescent serologic and polymerase chain reaction (PCR) testing
Diagnosis of tularaemia is suspected based on a history of contact with rabbits, hares, or rodents or exposure to arthropod vectors, the sudden onset of symptoms, and the characteristic primary lesion and regional lymphadenopathy.
Patients should have cultures of blood and relevant clinical material (eg, sputum, lesions); routine cultures may be negative, and the laboratory should be notified that tularemia is suspected so that appropriate media can be used and appropriate safety precautions are ensured.
Tularaemia has the following presentations:
- Ulceroglandular disease that presents with cutaneous ulcerations and marked lymphadenopathy
- Glandular disease that presents with no ulcers but marked lymphadenopathy
- Oculoglandular disease that presents with preauricular lymphadenopathy and conjunctivitis
- Oropharyngeal disease that presents with pharyngitis, stomatitis and cervical lymphadenopathy
- GI treat disease that presents with vomiting, abdominal discomfort, and diarrhea
- Respiratory disease that presents as pneumonia or pleuritis
- Typhoid tularaemia is a febrile illness without any early signs or symptoms
The risk of infection is increased in the following populations:
- Veterinarians
- Laboratory workers
- Farmers, landscappers
- People who work with animals, sheep
- People who handle meat
Prognosis
If tularaemia is not treated, it carries a mortality rate of 10-50%. Typhoid tularaemia carries the highest mortality. Even those who survive are left with residual scars, lung and kidney damage and muscle loss.
Complications
- Lung abscess, pneumonia
- ARDS
- Rhabdomyolysis
- Renal failure
- Meningitis
- Peritonitis
In short…
Tularaemia is defined as a zoonotic infection caused by the bacterium Francisella tularensis, which can lead to respiratory and non-respiratory clinical syndromes, including pneumonia and infected ulcers. It is primarily transmitted through contact with infected wild animals, particularly squirrels and rabbits.
As we continue with the story…
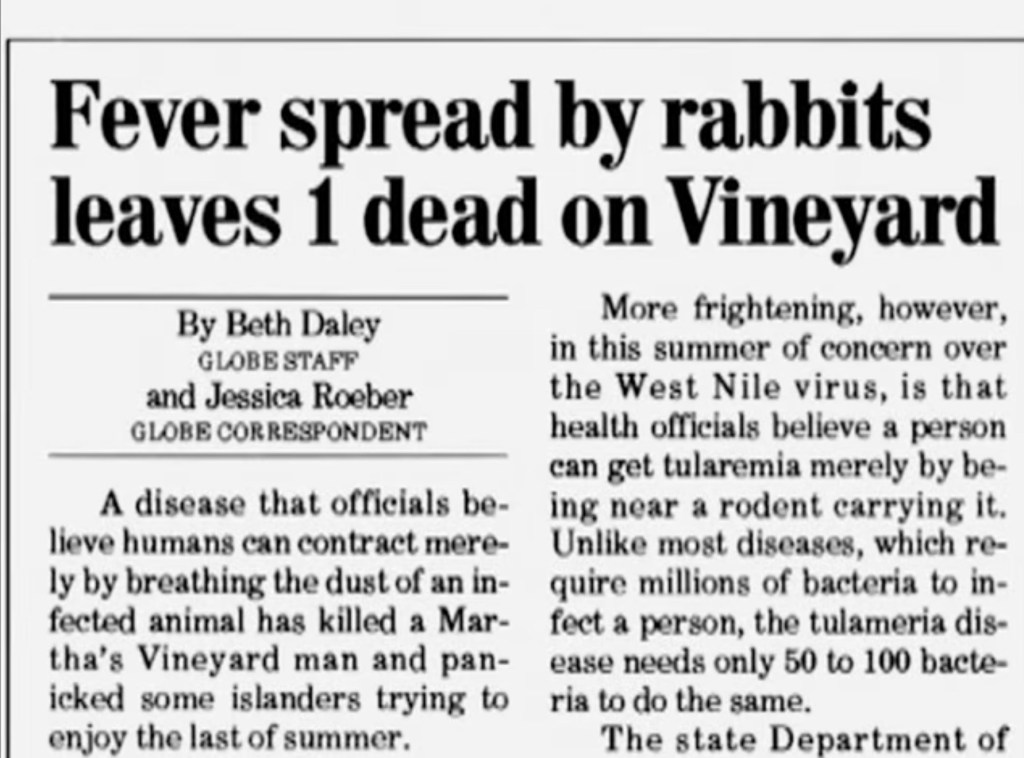
The discovery of the fourth patient Carter who was infected and that infection led to his passing. And this patient’s situation was caught up by the news. The clinical investigators (as well call the team that!) decided to do a case control study distributing questionnaires to patients who contracted tularaemia. They found a promising clue. “The only commonality was that most of these individuals worked in landscaping.” Nurse Donna explains. They went to talk to local landscapers looking for answers. The team went about the ‘whats’ of the occupational hazard that led them to contract the disease.
Public health officials issued an alert. Dr Bela Matyas, a Medical Epidemiologist and the one of the duo concerned on the matter who had notified the CDC during the initial progress of the outbreak says that everyone was doing their part to try and and get the word out.
Residents who now mow their lawns were to cover their mouths and hands, wear insect repellent at all times and avoid contact with dead animals. But they still weren’t sure where the disease came from. The location of exposure was a difficult find in one simple line to put it. Veterinarians reported nothing unusual. Next, the clinical investigators looked at wild animal populations across the island and more people began to get sick. By the end of August 2000, two months after the outbreak began, health officials were no closer to finding the source of the tularaemia outbreak. Doctors were concerned that the tourists might not get the right treatment for this sporadic infection rise in rates. Now, the clinical investigators were worried if this mysterious illness spread across the country. Then, the effects would be devastating.
Most of the cases of the tularaemia contracting seemed to have occurred in the southern part of the island. This was a less-developed part of the island and would explain the mysterious-ness of the nature of spread. CDC agents conducted an investigation, so now the idea according to Dr Telford is that the people involved in landscaping must be somehow inhaling the organism, but as to how it gets in the soil they really don’t know.
Suited up, they recreated the lawn mowing scene and collected the samples of grass and clippings. The bacteria samples were all negative. Their attention turned to the wild animals, it wasn’t going to be an easy catch! Or find!?
A skunk and a rat came back positive but all that means is that they were exposed to the pathogen!
When they thought the island was safe again, cases struck the island again, this time 11 of them and winter was fast approaching.
It was never recorded before that mowing lawns could be an activity that was associated with tularemia! And they were finally able to have some sort of findings to indicate that.
(All the names of the patients are changed as mentioned in the documentary for educational purposes).
Source:
diagnosis: UNKNOWN (Educational, informative TV show with a documentary edge!)
Documentary Vault
https://www.steamshipauthority.com/visitors/activities
https://www.ncbi.nlm.nih.gov/books/NBK430905/
https://www.msdmanuals.com/professional/infectious-diseases/gram-negative-bacilli/tularemia
https://www.sciencedirect.com/topics/medicine-and-dentistry/tularemia