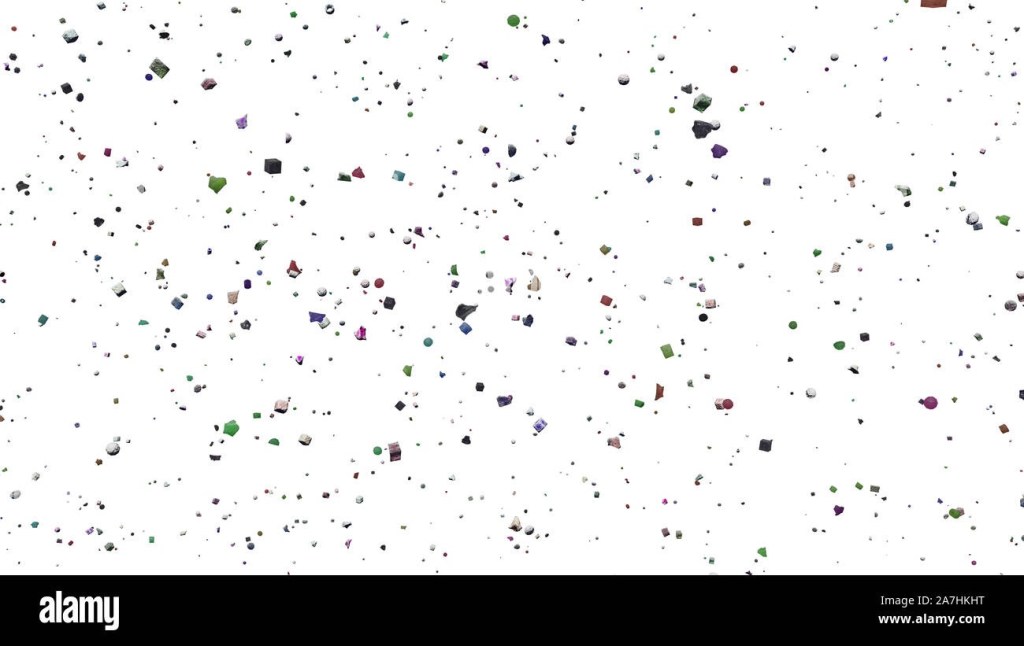
Plastic particle pollution is now prevalent in our ever-changing world. The journey of air pollution to the respiratory tract takes on a different perspective thanks to research. Plastic air pollution comes about depending on two consequences, microplastics and nanoparticles. Dr Suvash Saha and his team have recorded the areas of the respiratory system that are liable to damage and disease and the type of plastics that cause this.
Using computational fluid-particle dynamics (CFPD), the study was conducted to put emphasis on the transfer of particles and their location of impact based on its size and shape. The results are published in the journal Environmental Advances. Another important clue that the study would provide, is to create strategies that would get rid of potential risks and come up with beneficial health outcomes. Inhalation is deemed as the second most likely pathway for human exposure.
The primary source is the industry manufactured cosmetics and personal care products. The secondary source is the degradation of water bottles, food and clothes leading to fragmentation. Experimental evidence strongly suggests that exposure to these plastic particles can increase the potential susceptiblilty of human lung diseases. The UTS-University of Technology, Sydney modelling highlighted that faster breathing rates are correlated to the deposits in the upper respiratory tract and slower breathing rates are correlated to deeper lung tissue penetration. Particle shape being another factor of interest, non-spherical forms, showed a higher propensity of deposit, when it came to deeper lung penetration over spherical forms.
These findings will determine the assessments that can be used to evaluate the risk factors associated with respiratory exposure to nano and microplastic particles.
Nivea Vaz
Manipal College of Medical Sciences, Pokhara






Leave a comment