“Bukholderia pseudomallei is the causative agent of melioidosis. It found in the soil and water of tropical and subtropical regions globally. That being stated, there’s not much textual reference and representation of this disease in textbooks.”
Introduction
B. pseudomallei is a Gram-negative bacterium. Infection occurs following environmental exposure via percutaneous inoculation, inhalation or ingestion. Majority of cases are sporadic in nature with the minority being linked to contaminated products, water supplies and environments.
Most reported melioidosis cases occur in Southeast Asia and Northern Australia, the endemic area of coverage tends to expand, now covering Pacific, South Asia, Africa and the Americas. It is predicted that the incidence of melioidosis will increase proportionally as climate change increases. It’s endemic vastness has been indicated in southern USA, southeast Queensland part of Australia, and in close proximity with the La Niña phase of the El Niño-Southern Oscillation.
Melioidosis tends to be under-diagnosed in some endemic regions, due to limited access to laboratory diagnostics and lack of clinical knowledge. Low socioeconomic status is associated with the comorbidities that increase the risk for getting infected from the disease. This also increases the risk of dying from this disease!
The World Health Organisation affirms to make sure that melioidosis is not a neglected tropical disease. They have targeted at improving the melioidosis surveillance, awareness, diagnosis and management. This disease cannot be differentiated from community acquired infection by just clinical and radiology features, it requires much more.
Epidemiology
It arises from exposure of the host to bacteria, water or soil. Infection is through percutaneous exposure, inhalation, aspiration or ingestion. Diabetes is the most common risk factor for melioidosis. Other risk factors that are not limited to this disease are; hazardous alcohol consumption, chronic kidney disease, chronic lung disease, immunosuppressive therapy and thalassaemia with iron overload. Patients suffering from cystic fibrosis are advised to not travel or risk exposure to melioidosis endemic-prone areas.
Global Burden and Distribution
Melioidosis is highly endemic in Southeast Asia and Northern Australia, B.pseudomallei is common occurrence. Identification is done by using a simple laboratory algorithm with disc diffusion susceptibility testing to amoxicillin—clavulanate (susceptible), gentamicin (resistant), and colistin (resistant) was proven successful in Vietnam.
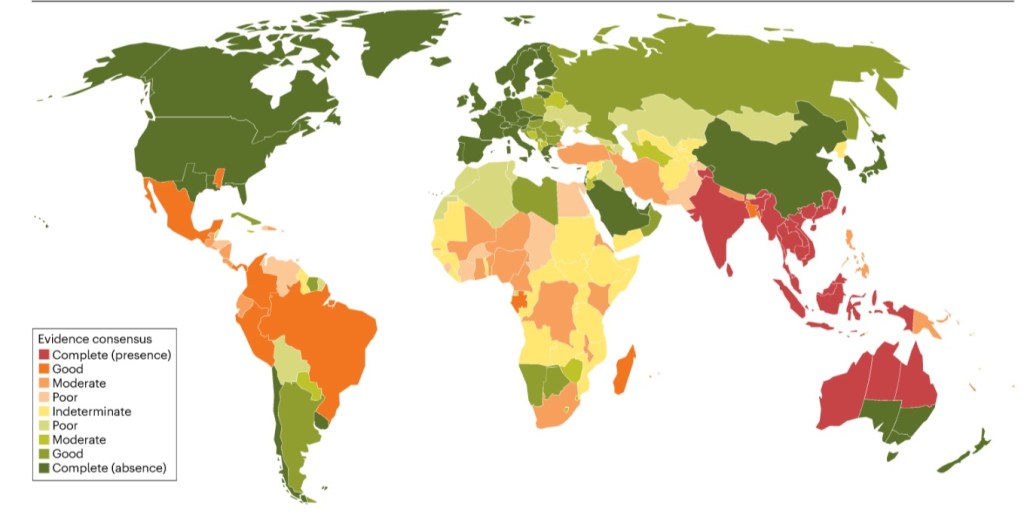
Global Distribution of Burkholderia pseudomallei.
The map represents the global distribution of B. pseudomallei based on a consensus evidence gathered from January 1910 to September 2022. Green colour represents complete consensus on the absence of B. pseudomallei and red represents complete consensus of B. pseudomallei.
Environmental niches, seasonality and climate
This microbe thrives in wet, acidic, low salinity, nutrient-deplete soil with low carbon levels. It can survive in desert and temperate environments for many years, and can grow in clayish soils composed of multiple layers of high porosity, showcasing its versatile adaptability.
It uses livestock and native animals in general as a vector of transport by means of rhizosphere that is found around the roots of grasses and around rice crops as well. It is no stranger to lurking around construction sites as well. Water has also been their means of transportation, with chlorination and ultraviolet being the only few ways of killing this microbe from water bodies. It’s movement in air has been detected during extreme weather conditions.
Pathophysiology
This bacterium has three types of type III secretion systems. The six types of type IV secretion systems confers the intracellular and survival ability in the microbe. It’s virulence factors include type III secretion systems, type IV secretion systems, two-partner secreting system, capsular polysaccharides, flagella, pili and adhesins.

Virulence factors of B. pseudomallei and host immune response
Signs & Symptoms
It is often mistaken for tuberculosis or pneumonia. According to the CDC, melioidosis has a wide range of signs and symptoms, it depends on the location of infection and which pathway precedes it:
~Localised infection-localised pain/swelling, fever, ulceration, abscess.
~Pulmonary infection-cough, chest pain, high fever, headache, and anorexia.
~Bloodstream infection-fever, headache, respiratory distress, abdominal discomfort, joint paint, disorientation.
~Disseminated infection-fever, weight loss, stomach/chest pain, muscle/joint pain, headache, central nervous system/brain infection, seizures.
Diagnosis, treatment and prevention
Isolation and culture of B. pseudomallei is the gold standard method of diagnostics. Clinical specimens are blood cultures, sputum, urine and depending on site sterility can include swabs, pus and fluids. Throat and rectal swabs can replace sputum sample if there’s a difficulty in obtaining it, provided it is done is selective liquid media. B. pseudomallei are small, creamy and have a metallic sheen, subsequently becoming dry and wrinkled; on Ashdown medium, a purple colour is obtained. It is a Gram-negative rod bacterium, with bipolar staining, giving it a safety pin appearance, and is oxidase-positive and indole-negative. Latex agglutination with monoclonal antibodies against B. pseudomallei exopolysaccharide is a useful bench test to aid identification.
Research on the antimicrobial effectiveness based on clinical minimum inhibitory concentration (MIC) and zone diameter breakup points against this microbe is successful. Higher doses of ceftazidime, trimethoprim, sulfomethoxazole, doxycycline, amoxicillin, clavulanate are required for bactericide effects.
Treatment
Therapy begins with an intensive phase of a minimum of 10-days of intravenous ceftazidime or carbapenem, with or without trimethoprim-sulfamethoxazole. This is followed by an eradication phase of oral trimethoprim-sulphamethoxazole for 3-6 months. In very specific cases, such as those involving a single skin lesion without bacteraemia or sepsis, an oral only regimen of trimethoprim-sulfamethoxazole has been used. Surgical drainage of large abscesses is indicated but usually is not required for multiple small liver and splenic abscesses. Prostate abscesses usually require drainage, done by trans-rectal ultrasound guidance.
Prevention
In Thailand, evidence based guidelines for the prevention of melioidosis, recommends that the residents, rice farmers and visitors should wear protective gear, like boots and gloves, when coming in contact with water, or soil, as exposure should be avoided. This includes outdoor exposure to heavy rains and dust clouds. The guidelines also encourage cessation of smoking and discourage the application of herbal remedies. And drinking bottled water or boiled water is a must.
Vaccines are currently underway for this mortifying bacterium!
The International Melioidosis Network is a forum dedicated to finding information, sharing experiences and detailing new findings in research!
Nivea Vaz
Manipal College of Medical Sciences, Pokhara






Leave a comment