‘An Unusual Loss of Consciousness’
A panic sounding voice on the phone exclaimed, “I can’t wake my wife up!” The woman, his wife of 43 years began to snore. This was not something she’d done before. As her husband, he tried to wake her up. He just didn’t get it. He had a fit and healthy wife.
The day started off quite normal, she was healthy and active, and got home from work as usual in the late afternoon, made dinner and went for her kickboxing class. After that, she had got home, put the children to sleep and had a drink: a mix of vodka and cranberry juice. The couple went to bed. Normally, the husband would be up and his wife would go to sleep comparatively early but today they went to sleep together. As they were talking the wife began to snore which was unexpected, so much so that he thought his wife was joking around with him. Her husband tried to wake her but it was of no use, he shouted her name, shook her shoulder. He was now terrified and dialled up 911.
It was up to the medics to wake her up, they called her name, they administered her Narcan, a counteractive drug for narcotics even though her husband mentioned with the utmost surety that she doesn’t take any drugs. All the response that they had got from her was a moan, she was briskly loaded inside the ambulance that drove her to the ER of the University of Michigan Medical Centre. Dr Robert Silbergleit was the doctor on duty that night. The EMTs would report her as a “Comatose, forty-three-year-old woman found by her husband, she’s snoring and unresponsive except to pain.” He noted that the patient was perfectly fit and healthy albeit asleep. He rubbed her chest using the sternal rub manoeuvre. “Stop” she moaned but she didn’t open her eyes and she didn’t wake up.
Dr Silbergleit listed down mentally the possible causes of her strange and unexpected somnolence. Drug overdose-he sent off the blood and urine samples to detect sedating drugs or alcohol, traumatic brain injury-had she been hit in the head during kickboxing class? If so, that would mean a possible brain injury so an inquiry for a CT scan was done, stroke-the sudden onset of symptoms sounded like a stroke but the sudden loss of consciousness didn’t, still, stroke had to be considered because it can be reduced or even prevented by medications. The drugs though had to be given within four and a half hours of the onset of symptoms because these drugs had the potential to cause life-threatening bleeding.
Ischemic stroke usually results when an artery to the brain is blocked, often by a blood clot and/or a fatty deposit due to atherosclerosis. Symptoms occur suddenly and may include muscle weakness, paralysis, lost or abnormal sensation on one side of the body, difficulty speaking, confusion, problems with vision, dizziness, and loss of balance and coordination. Diagnosis is usually based on symptoms and results of a physical examination and brain imaging. Other imaging tests (computed tomography and magnetic resonance imaging) and blood tests are done to identify the cause of the stroke.
Results; the drug tests were negative, the blood-alcohol level were consistent with the reported single dinner drink, and the CT scan didn’t show evidence of bleeding or a stroke. Silbergleit ordered a CT angiogram- outlining the brain with the arteries for any suggestive of a stroke. It appeared normal. The doctor spoke to Lesli Skolarus, a neurologist specialised in strokes. He explained to him that he was planning to get his hands on an EEG to see if the woman was having continuing seizures. The neurologist was at home and he had to hurry to the hospital, arriving at around 1:00 a.m. By the time, Skolarus finished reviewing the results, her patient fell asleep and two hours had passed since.
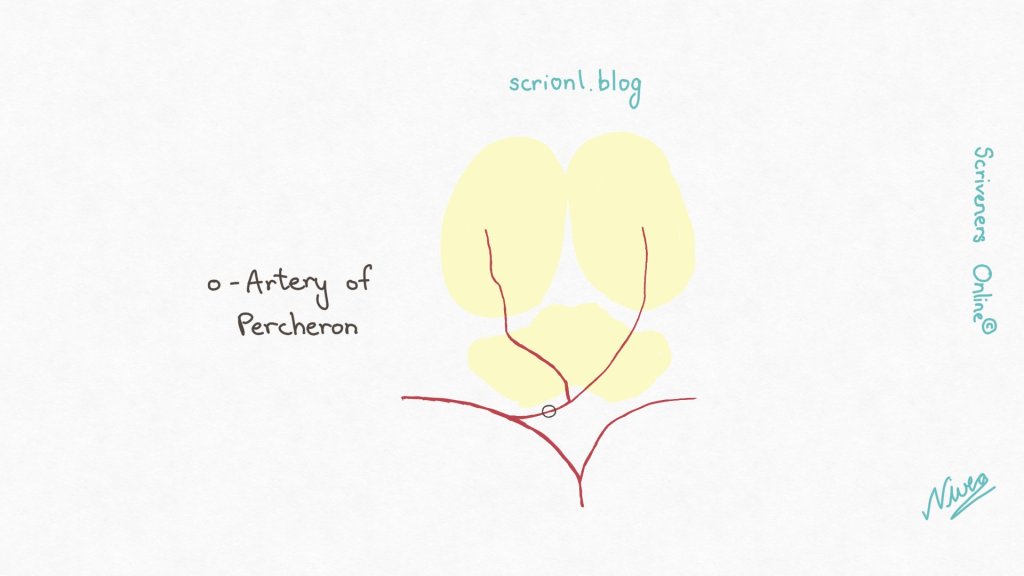
Artery of Percheron territory infarct is rare, on account of the relative rarity of the artery of Percheron, and presents with a variety of signs and symptoms collectively termed the paramedian thalamic syndrome. It is a type of posterior circulation infarction. On imaging, it is classically characterized by bilateral infarcts in areas involving the rostral midbrain and/or ventromedial thalamus. Artery of Percheron territory infarcts are thought to account for 4-18% of all thalamic ischemic strokes.
Treatment may include medications to break up blood clots or to make blood less likely to clot and procedures to physically remove blood clots, followed by rehabilitation. About one third of people recover all or most of normal function after an ischemic stroke. Preventive measures include control of risk factors, medications to make blood less likely to clot, and sometimes surgery or angioplasty to open blocked arteries.
She was struck as much as the ER doctor was with the sudden onset of symptoms. Was it even a stroke? If its was, it was an odd one. Any obstruction in this case will cut off blood and oxygen supply to the brain. The typical stroke she’s studied on would cause weakness or paralysis on one side of the body, keeping the patient wide awake. The part of the brain keeping us awake is the RAS (Reticular Activating System). One artery on each side of the brain feeds the RAS, in case one was blocked it would give protection.
Causes of Ischaemic Stroke
An ischemic stroke typically results from blockage of an artery that supplies blood to the brain, most commonly a branch of one of the internal carotid arteries. As a result, brain cells are deprived of blood. Most brain cells die if they are deprived of blood for 4.5 hours.
Common causes
Commonly, blockages are blood clots (thrombi) or pieces of fatty deposits (atheromas, or plaques) due to atherosclerosis. Such blockages often occur in the following ways:
- By forming in and blocking an artery
- By travelling from another artery to an artery in the brain
- By travelling from the heart to the brain
Blood clots in a brain artery do not always cause a stroke. If the clot breaks up spontaneously within less than 15 to 30 minutes, brain cells do not die and people’s symptoms resolve. Such events are called transient ischemic attacks (TIAs).
If an artery narrows very gradually, other arteries (called collateral arteries) sometimes enlarge to supply blood to the parts of the brain normally supplied by the clogged artery. Thus, if a clot occurs in an artery that has developed collateral arteries, people may not have symptoms.
The most common causes of ischemic stroke can be classified as
~Cryptogenic stroke
~Embolic stroke
~Lacunar infarction
~Large-vessel atherosclerosis (the 4th most common cause)
However, a small segment of the population has only one vessel delivering blood to the RAS and a well-positioned clot to this single vessel called the artery of Percheron could completely block flow to the RAS and in turn cause consciousness. Skolarus had seen this stroke during her training years in an elderly man who had lost consciousness, but by the time they discovered it, the damage had been permanent.
Skolarus looked at the clock, it’s been three hours that had passed since the start of the woman’s symptoms. If she really had a clot in the artery of Percheron, there was still time to use a clot buster to re-open the vessel. But to perform this, they would require an MRI. A half an hour later, Skolarus watched as the midbrain imaging appeared in front of her. A bright red spot was visible indicating a clear damage to the artery of Percheron, she called the ER to get the drug busting clot ready.
Many different symptoms can occur, depending on which artery is blocked and thus which part of the brain is deprived of blood and oxygen (see Brain Dysfunction by Location).
When the arteries that branch from the internal carotid artery (which carry blood along the front of the neck to the brain) are affected, the following are most common:
~Blindness in one eye
~Loss of vision on either the left side or the right side of both eyes
~Abnormal sensations, weakness, or paralysis in one arm or leg or on one side of the body
~When the arteries that branch from the vertebral arteries (which carry blood along the back of the neck to the brain) are affected, the following are most common:
~Dizziness and vertigo
~Double vision or loss of vision in both eyes
~Generalized weakness on one or both sides of the body
~Many other symptoms, such as difficulty speaking (for example, slurred speech), impaired consciousness (such as confusion), loss of coordination, and urinary incontinence, can occur.
~Severe strokes may lead to stupor or coma. In addition, strokes, even milder ones, can cause depression or an inability to control emotions. For example, people may cry or laugh inappropriately.
~Some people have a seizure when the stroke begins. Seizures may also occur months to years later. Late seizures result from scarring or materials that are deposited from blood in the damaged brain tissue.
~Occasionally, fever develops. It may be caused by the stroke or another disorder.
~If symptoms, particularly impaired consciousness, worsen during the first 2 to 3 days, the cause is often swelling due to excess fluid (edema) in the brain. In large strokes, the swelling in the brain is typically at its worst about 3 days after the stroke begins. Symptoms usually lessen within a few days, as the fluid is absorbed. Nonetheless, the swelling is particularly dangerous because the skull does not expand. The resulting increase in pressure can cause the brain to shift, further impairing brain function, even if the area directly damaged by the stroke does not enlarge. If the pressure becomes very high, the brain may be forced sideways and downward in the skull, through the rigid structures that separate the brain into compartments. The resulting disorder is called herniation, which can be fatal.
The medication started before the four and a half hours deadline. As the medicine was dripping in, she showed the patient’s husband the scans. Then, she told the bad news the fact that she might never wake up. Even she did there would be damage. Suddenly the husband heard his wife’s voice, he rushed with Skolarus to the bedside, she was scared but her eyes were open and she was talking.
Complications of stroke
Strokes can lead to other problems (complications):
~If swallowing is difficult, people may not eat enough and become malnourished and dehydrated.
~Food, saliva, or vomit may be inhaled (aspirated) into the lungs, resulting in aspiration pneumonia.
~Being in one position too long can result in pressure sores and lead to muscle loss, deconditioning, urinary tract infections, and permanent shortening of muscles (contractures).
~Not being able to move the legs can result in the formation of blood clots in deep veins of the legs and groin (deep vein thrombosis).
~Clots in the deep veins of the legs can break off, travel through the bloodstream, and block an artery to a lung (a disorder called pulmonary embolism).
~People may have difficulty sleeping.
~The losses and problems resulting from the stroke may make people depressed.
She knew her name, his name, and the name of the current president, she was back.
She stayed in the hospital for the next several days, the doctors wanted to know why all of this was happening to her. A sonogram of the heart gave them the answer to their question. There was an opening in the heart wall that separated the right side from left side. The clot most likely travelled from the lung through the heart to the brain. When the author of this book, spoke to her, she mentioned that she was back to her old self and was amazed and grateful.
“There were so many ways I was lucky that night. If my husband had come to bed at his usual time, he might have not noticed anything. If the neurologist hadn’t come in, if the MRI hadn’t been available…” She stopped. “It’s all a little scary.”
(ps: I had to do a re-post cause I had to re-upload my illustration!)
Source;
Diagnosis: Solving the Most Baffling Medical Mysteries-Lisa Sanders. (Cases go in no particular order!)
https://www.msdmanuals.com/home/brain-spinal-cord-and-nerve-disorders/stroke/ischemic-stroke
https://radiopaedia.org/articles/artery-of-percheron-territory-infarct






Leave a comment